Gynecologic Cancers and Weak Pelvic Floor

Women with gynaecological cancers can experience weak pelvic floor following cancer treatment. Guest doctor Dr Yap Lip Kee explains more about what it is, and how it can be managed.
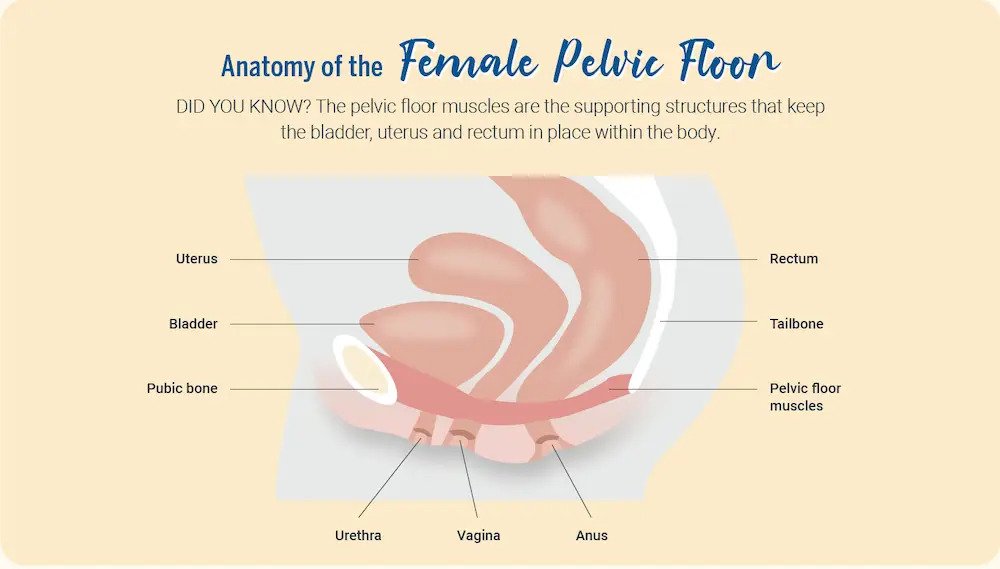
The pelvic floor is a group of muscles found at the base of the pelvis. It comprises three main layers of muscles that extend from the pubic bone to the tailbone.
When the muscles of the pelvic floor work together, they perform several important functions in the body, such as bladder, bowel, and sexual function, as well as spinal stability.
However, this may not always be the case for individuals with cancer, such as gynaecological cancers (which include endometrial, ovarian, and cervical cancers). Gynaecological cancers and their subsequent treatments can have a big impact on pelvic floor function, and lead to a weak pelvic floor, or pelvic floor dysfunction.
What is pelvic floor dysfunction?
Pelvic floor dysfunction refers to an inability to relax and coordinate the pelvic floor muscles to have a bowel or bladder movement. It may commonly present as:
- Urinary incontinence (leakage)
- An overactive bladder (frequent urge to pee)
- Bowel incontinence (leaking stools)
- Incomplete emptying of stools
- Constipation
- Pelvic organ prolapse
Pelvic organ prolapse tends to be the most visible and distressing manifestation of pelvic floor dysfunction, although not the most common.
Other symptoms include pelvic pain and pressure, as well as pain during sex. However, these symptoms are not commonly associated with pelvic floor dysfunction.
Impact of pelvic floor dysfunction on the body
To demonstrate the impact of pelvic floor dysfunction on important body functions, picture the pelvis as the home to pelvic organs such as the bladder, uterus and rectum.
The pelvic floor muscles are the supporting structures that keep everything in place within the body. This is because the pelvic floor muscles are attached to the pelvic bone and give stability to the pelvic organs by forming a sling around the rectum.
Now picture what happens when the supporting structures are weakened or disabled.
When the pelvic floor muscles are too relaxed or loosened, the bladder and urethra (i.e. the tube leading from the bladder to the urethral opening, through which urine leaves the body) are unable to hold back urine, leading to incontinence. Similarly, loose muscles supporting the rectum may lead to the risk of leakage of stools.
Conversely, when the pelvic floor muscles are too tense or tightened around the bladder and urethra, it may lead to an increased frequency of micturition, or an increased need (or sensation of need) to pee. Tense or tight muscles around the rectum can also cause difficulty in releasing stools, which may express as constipation, the inability to defecate, or a constant sensation of needing to defecate but an inability to do so.
Causes of pelvic floor dysfunction
Pelvic floor dysfunction may occur after cancer treatment, when the pelvic floor muscles and ligaments are impaired.
Surgery for gynaecological cancers, for instance, can cause marked weakening and displacement of the muscles and ligaments of the pelvis. It includes surgical procedures such as:
- Tumour debulking
- Bowel resection
- Partial or complete bladder removal - Organ removal
- Hysterectomy (removal of the uterus)
- Salpingo-oophorectomy (removal of the fallopian tubes and ovaries)
Chemotherapy and radiation therapy can also lead to fibrosis, or hardening, of the pelvic floor muscles. This can in turn lead to a shortening or narrowing of the vaginal canal. The usual sequelae of this condition is urinary incontinence, pelvic pain and sexual dysfunction (mainly pain during intercourse, as well as loss of sensation and response to sexual stimulus).
Pelvic floor dysfunction is fairly common among gynaecological cancer patients. More than half of women with gynaecological malignancies experience urinary incontinence, while 10%–30% of women undergoing radical surgery have experienced a pelvic organ prolapse. In addition, easily half of gynaecological cancer survivors complain of a reduction in quality of life as a result of weak pelvic floor.
Managing weak pelvic floor
While there is much emphasis on healing and strengthening pelvic floor muscles after pregnancy and childbirth, there is little emphasis on managing pelvic floor dysfunction after gynaecological cancer treatment.
Fortunately, there are ways to manage a weak pelvic floor resulting from gynaecological cancers and their subsequent treatments.
Some methods of relieving symptoms of pelvic floor dysfunction include physical therapy, biofeedback therapy and medications. In general, a combination of physiotherapy and techniques to strengthen pelvic floor muscles can aid patients in restoring normal pelvic floor function.
As a start, your doctor may assess your history of pain, symptoms, bowel and bladder functions, diet composition, biopsychosocial factors, occupation, stress levels, pregnancy history, trauma, and medications. This should be followed by a postural examination, both standing and sitting.
Subsequently, a pelvic floor assessment that includes an external and internal examination of the vagina and/or rectum should be carried out. Your doctor should take note of the skin and external musculature of the perineum, and address issues such as skin irritation and external pelvic floor atrophy or asymmetry.
After a comprehensive evaluation, your doctor can recommend an individualised treatment programme to help you manage your condition.
If you experience any symptoms of pelvic floor dysfunction following gynaecological cancer treatment, know that they can be addressed. Speak to your oncologist and gynaecologist, or visit an experienced physiotherapist who can guide you through returning to optimal pelvic floor health.
Gynecologic Cancers and Weak Pelvic Floor originally appeared on Parkway Cancer Centre
and has been republished with permission
Further Reading
The article above is meant to provide general information and does not replace a doctor's consultation.
Please see your doctor for professional advice.
