Coronary Heart Disease
Coronary Heart Disease (CHD), also known as Coronary Artery Disease (CAD) builds up over many years and can lead to angina, heart attacks and sudden cardiac arrest. CHD is the result of plaque buildup in the coronary arteries - a condition called atherosclerosis, and this leads to blockage of these arteries. The heart muscles thus become starved of oxygen and the vital nutrients it needs to function properly.
Your Amazing Heart
 Your heart is an amazing organ which is constantly working, pumping blood around your body, from cradle to grave. It contracts and relaxes up to 100,000 times a day, without you being even conscious of it.
Your heart is an amazing organ which is constantly working, pumping blood around your body, from cradle to grave. It contracts and relaxes up to 100,000 times a day, without you being even conscious of it.
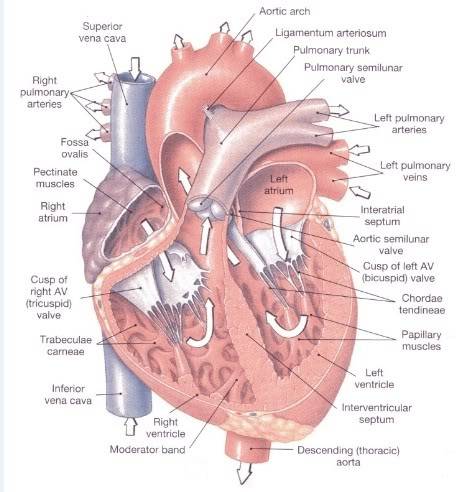
The basic function of the heart is to pump oxygenated blood and nutrients through arteries to the tissues of the body. When the oxygen and nutrients have been extracted by the tissues, the veins carry blood back to the heart.
There are 2 sides to the heart, each of which acts like a separate pump. The two sides and each sub-divided into 2 separate chambers, making a total of 4 chambers in all - the right and left atria, and the right and left ventricles. The upper chambers (the atria) act like collecting reservoirs, whilst the lower chambers (the ventricles) are more muscular as they function as the pumping stations, to pump blood out of the heart. The right side of the heart collects de-oxygenated blood from the body and pumps it to the lungs in order to get oxygenated. The left side of the heart collects oxygenated blood from the lungs, and pumps it to the rest of the body.
In order for the blood to reach the various organs and tissues in the body, blood is pumped at very high pressures. Also, as the heart needs to beat constantly, it does not fatigue, unlike the skeletal muscles. It is also essential that the heart muscles receive a very good blood supply in order to function well, and this is provided for by the coronary arteries.
The right and left coronary arteries branch off the aorta as it leaves the heart. They run across the surface of the heart and send off smaller vessels which penetrate into the myocardium (heart muscle) supplying richly oxygenated blood to it. Blood can flow through these vessels into the myocardium only between beats, as the heart relaxes. While the heart is in a contracted state, the pressure is too great to allow any blood to pass through. Hence, the heart requires a very efficient network of fine blood vessels within the myocardium, to get blood to where it is needed.
What Goes Wrong?
In coronary heart disease, the coronary arteries become narrowed (most often due to atheroma plaque build up), and the heart muscles become starved of the blood and oxygen it needs. At rest, this may not matter, but when your heart needs to work harder, such as during exercise, the coronary arteries may not be able to keep up the oxygen demand, and you may experience chest pain (known as angina). If blood supply to a portion of the heart muscle is blocked completely, or if the energy demands of the heart become much greater than its blood supply, a heart attack (injury to the heart muscle) may occur.
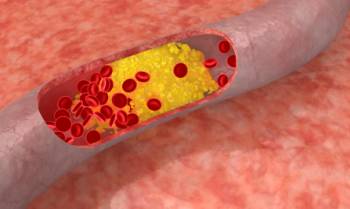
Atheroma Formation:
Atherosclerosis is a condition in which fatty material builds up along the walls of the arteries. Eventually, this build-up leads to hardening and narrowing of the arteries. It is a silent and progressive disease which blocks the arteries over time.
The extent and rate at which atheromatous plaques build up are affected by the level of fats (in particular, LDL-cholesterol) in the blood. People who have higher blood LDL levels are more likely to develop atheroma.
As patches of atheroma grow, they thicken and weaken the wall of the artery and gradually reduce the flow of blood through it. The distribution of these atheroma plaques is curiously patchy throughout the body. So, the narrowing may affect one coronary artery, but not another. It may also just affect one part, or can affect the artery throughout its length. This is of importance to the cardiologist, who will need to decide on the most suitable treatment.
In coronary heart disease, you may hear the terms: "single-vessel", "double-vessel" or "triple-vessel" disease. This basically refers to the number of branches of the coronary arteries, which are affected (the two main branches of the left coronary artery, and the right coronary artery).
Thrombus Formation:
The inner lining of our arteries is normally smooth and does not provide any focus on which clots can form. When atheroma develops, this lining is no longer smooth. Furthermore, a plaque is like a firm shell with a soft inner core containing cholesterol. As blood hits it during each heartbeat, the plaque may crack open and expose its inner cholesterol core, which promotes blood clotting.
Such thrombus from a plaque rupture will generally cause a sudden compromise in blood supply. This is the typical cause of a heart attack.
What Are The Risk Factors?
There doesn't seem to be any single cause for coronary heart disease. Rather, there are a whole range of things that make you more likely to develop CHD. The following are some of the risk factors for CHD:
• Age - the older you are, the higher your risk
• Sex - males are at greater risk of developing coronary heart disease, but women start to catch up after menopause.
• Genetics - if your father suffered a heart attack below the age of 60, or your mother below the age of 65, you would be considered to be at increased risk.
• Smoking
• Uncontrolled hypertension
• High blood cholesterol - high blood cholesterol levels make the build-up of plaques and consequent atherosclerosis more likely. High cholesterol can be caused by high LDL-cholesterol ("bad cholesterol) levels or low HDL-cholesterol ("good" cholesterol) levels.
• Diabetes - both Type I and Type II diabetes increase the risk of CHD. Diabetics may present with non-typical symptoms of CHD.
• Obesity - obese people have a higher risk of developing coronary heart disease.
• Lack of exercise - people who lead very sedentary lives have a higher risk of developing coronary heart disease.
• C-reactive protein (CRP) - studies have found that CRP concentration is associated with an increased risk of a wide range of diseases, including: heart attacks, stroke, deaths from various cancers, chronic lung disease, injuries, and other conditions.
• Fibrinogen - fibrinogen is a blood protein which is involved in blood clotting. Excess levels may encourage the clumping of platelets, resulting in the formation of clots.
• Homocysteine - CHD, as well as some other cardiovascular conditions have been found to more likely to occur if homocysteine levels are elevated.
• Lipoprotein (a) - may undermine the body's ability to dissolve blood clots. Lipoprotein (a) forms when an LDL particle attaches to a specific protein.
Recognizing The Symptoms
1. CHEST PAIN
The most common symptom of coronary artery disease is angina, or chest pain.
Not all chest pain is cardiac in origin. Other causes of chest pain may be muscular in origin, or due to acid regurgitation. Sometimes, distinguishing cardiac pain from other causes of chest pain can be difficult, even for experienced doctors.
Angina pectoris is Latin for "pain in the chest". It is typically brought on by exertion, such as climbing up a flight of stairs, and goes away with rest. It typically lasts no more than 10 minutes. The pain is brought on when the cardiac muscle fibres do not receive sufficient oxygen for the work that they are doing.
Unstable Angina describes increasing angina in previously diagnosed angina, which has become more frequent, longer in duration, or precipitated by less exercise within the past two months, and angina occurring at rest, usually of more than twenty minutes duration, experienced within the past week. It is caused by disruption of an atherosclerotic plaque in the coronary arteries with partial thrombosis and possibly embolization or vasospasm.
It represents a severity of CHD between stable angina pectoris and a heart attack (myocardial infarction).
In a Heart Attack (myocardial infarction), the pain is similar to angina, but it persists even with rest. There are often associated symptoms, such as profuse sweating, shortness of breath, nausea, vomiting, palpitations, and anxiety (often described as a sense of impending doom). Someone experiencing a heart attack will often feel cold and clammy.
The difference between angina and a heart attack is that, whilst angina leaves the heart muscle short of oxygen but basically undamaged, in a heart attack, the disruption to oxygen supply is so acute and severe, that part of the heart muscle actually dies.
2. PALPITATIONS
Palpitations are said to occur when the heart beats irregularly, beats faster or stronger, or misses a beat. Palpitations may occur with CHD, but may also be brought on by stress, smoking, alcohol or by drinking too much coffee or tea.
3. BREATHLESSNESS
There are many causes of breathlessness, such as asthma, bronchitis, and even anxiety. Heart failure also causes breathlessness and can affect someone who has had a heart attack. After a heart attack, the heart can sometimes be in a "stunned" state, or part of the wall is unable to function properly. Hence, the heart is unable to pump properly and fluid may build up in the tissues and lungs, resulting in breathlessness. You may then find it difficult to lie flat in bed or wake up in the middle of the night with problems catching your breath. You may also develop a cough with frothy or slightly blood-stained sputum.
In heart failure, fluid often also builds up in the legs, causing them to swell especially after prolonged standing or walking.
How Is CHD Diagnosed?
Your doctor will make the diagnosis of coronary artery disease by:
• Talking to you about your symptoms, medical history, and risk factors.
• Performing a detailed physical exam.
• Performing several diagnostic tests to help evaluate the extent of your coronary heart disease, its effect on the function of your heart and the best form of treatment for you. These may include a resting ECG, exercise ECG (treadmill test), radioactive isotope tests, stress echocardiography, coronary angiogram etc.
How is CHD Treated?
Treatment for coronary artery disease involves making the necessary lifestyle changes, taking medications, and possibly undergoing invasive and/or surgical procedures. You will also need to be on regular follow-up by your doctor/cardiologist.
• Reduce your risk factors:
Quit smoking, if you smoke. Maintain a healthy diet, low in fats, cholesterol and salt but high in wholegrains, fruits and vegetables. Keep your blood sugar under control if you have diabetes, and ensure that your blood pressure is well controlled. Exercise regularly (but talk to your doctor before you starting an exercise program), and try to maintain a healthy weight.
• Medication:
Medications are often prescribed to help your heart work more efficiently and receive more oxygen-rich blood. The drugs you need will depend on you and your specific heart problem. Drugs are also given to control hypertension, hypercholesterolaemia and diabetes (if present).
• Surgery and other procedures:
Common procedures to treat coronary artery disease include balloon angioplasty (PTCA) with or without stent placement, and coronary artery bypass surgery (CABG). All of these procedures help increase the blood supply to the myocardium, but it is important to ensure that you decrease your risk factors to prevent re-blocking (ie. re-stenosis) of the coronary arteries.
Further Reading
The article above is meant to provide general information and does not replace a doctor's consultation.
Please see your doctor for professional advice.