Obstructive Sleep Apnoea
 Sleep apnoea is a common disorder in which there are one or more "apnoeic" (paused breathing) episodes during sleep. These apneoic episodes may last several seconds to minutes, occurring as often as 5 to 30 times or more in an hour. After this period of apnoea, the sufferer often chokes or snorts, before returning to normal breathing. As such, the patient with sleep apnoea typically moves in and out of deep sleep throughout the sleep period, resulting in poor sleep quality and daytime fatigue. Severe sleep apnoea may be life threatening if left untreated.
Sleep apnoea is a common disorder in which there are one or more "apnoeic" (paused breathing) episodes during sleep. These apneoic episodes may last several seconds to minutes, occurring as often as 5 to 30 times or more in an hour. After this period of apnoea, the sufferer often chokes or snorts, before returning to normal breathing. As such, the patient with sleep apnoea typically moves in and out of deep sleep throughout the sleep period, resulting in poor sleep quality and daytime fatigue. Severe sleep apnoea may be life threatening if left untreated.
It has been estimated that between 40-60% of men and 30-40% of women snore. Snoring results from the partial obstruction of the upper airway during sleep. The tendency to snore increases with age, and there is a spectrum of snoring, from mild snoring (which is harmless) to obstructive sleep apnoea (which should be treated).
Most people with sleep apnoea are unaware that they have the condition because it occurs only during sleep. Hence, it requires a high index of suspicion on the part of the doctor, to pick up possible sleep apnoea, and order further investigations to confirm it.
Awareness about the condition often also helps bring patients to see their doctors about it.
Classification
There are 3 forms of sleep apnoea: (i) obstructive sleep apnoea (OSA), (ii) central sleep apnoea (CSA) and (iii) mixed sleep apnoea (a combination of OSA and CSA).
In CSA, the central neurological controls for breathing malfunction; in OSA, breathing is interrupted by a physical block to airflow despite normal respiratory effort.
Obstructive Sleep Apnoea (OSA), is by far, the most common type of sleep apnoea. During sleep, muscle tone normally relaxes. When this happens at the level of the upper airways, normal airflow can become obstructed, causing apnoea. During these apnoeic episodes, there is an actual drop in blood oxygen saturation levels. Symptoms of OSA include daytime fatigue/sleepiness, restless sleep and loud snoring (interspersed by periods of apnoea followed by gasps). Other symptoms may include changes to mood (eg. irritability, depression, anxiety), forgetfulness, poor concentration, low sex-drive etc.
Risk factors for OSA:
With aging, there is a general decrease in muscle tone and laxity of supporting structures. As such, the elderly are at higher risk for OSA. Men, compared to women, tend to have an increased neck and torso mass, making them more prone to developing OSA. Women, during pregnancy and after menopause, are also at increased risk.
Smoking may also increase the risk of developing OSA. Decreased muscle tone may be caused by alcohol or the consumption of certain medication. Those with excessive soft tissue around the airway (eg. because of obesity), or those with structural features (eg. enlarged tonsils or adenoids) that narrow the airway, are at higher risk for developing OSA.
Patients with diabetes also are up to about 3 times more likely to develop OSA.
Complications of OSA:
Daytime sleepiness caused by OSA can significantly increase the risk of accident-related injuries. Left untreated, OSA is a major risk factor for road and industrial accidents.
A number of cardiovascular diseases have an association with obstructive sleep apnoea. These include high blood pressure, heart failure, heart arrhythmias and stroke. The association may be because these cardiovascular diseases and OSA, both have obesity as a common cause. However, several large studies have suggested that OSA itself, independent of obesity, may lead to or worsen cardiovascular diseases.
Diagnosis of OSA:
 OSA is often underdiagnosed because it cannot be simply detected by a routine visit to the doctor, or via a blood test. A high index of suspicion is required, based on reported symptoms and physical examination. Your doctor will ask you about symptoms of daytime sleepiness, and will probably need to speak to your family members or bed partner about whether or not your snore, and if so, how loudly you snore and if there are periods when breathing seems to stop followed by a gasping or choking sound.
OSA is often underdiagnosed because it cannot be simply detected by a routine visit to the doctor, or via a blood test. A high index of suspicion is required, based on reported symptoms and physical examination. Your doctor will ask you about symptoms of daytime sleepiness, and will probably need to speak to your family members or bed partner about whether or not your snore, and if so, how loudly you snore and if there are periods when breathing seems to stop followed by a gasping or choking sound.
Your doctor will then check your BMI (those who are obese are at increased risk for OSA), examine your mouth, nose and throat for extra or enlarged tissue. An enlarged tonsils, floppy uvula and low-lying soft palate can all predispose one to OSA.
If your doctor feels that OSA is likely, he may refer you to see a specialist, or order a sleep study.
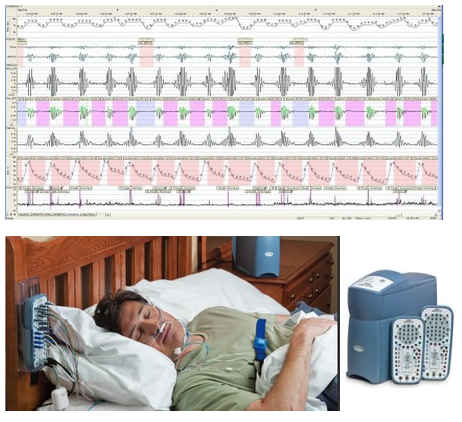
A sleep study is the most accurate test used to diagnose sleep apnoea. In the past, sleep studies (the polysomnogram) had to be done in a hospital setting (at the so-called "sleep labs" or "sleep centres"). The polysomnogram records brain activity, eye movement, breathing, heart rate, blood pressure, blood oxygenation etc whilst you sleep. It is a painless procedure, but there are obvious disadvantages eg. cost of staying overnight at the sleep centre, unfamiliar surroundings which can make sleep difficult etc.
Fortunately, home-based sleep study monitors are now available, and are being used more extensively by specialists and general practitioners to aid in the diagnosis of sleep apnoea. They may also be used for home titration of positive airway pressure (PAP) treatment. The advantages of portable monitoring include its convenience (can be performed at home) and the lower cost compared to polysomnography. However, a disadvantage is that fewer physiological variables are measured by the portable system, which can potentially lead to misinterpretation. If the results are inconclusive, patients may still require formal polysomnography testing.
Management of OSA:
There are a wide variety of treatment options for OSA, depending on the cause of the the obstruction as well as the severity of obstruction.
Lifestyle changes:
Losing weight, avoidance of alcohol and smoking, avoidance of medication which relax the central nervous system (eg. muscle relaxants and sedatives) can help eleviate some of the obstruction. Special pillows and oral appliances may also help keep the airway open during sleep. Sleeping at a 30 degree elevation of the upper body and sleeping on the side (as opposed to lying supine) have been shown to be helpful as well.
Positive Airway Pressure:
Positive airway pressure is the most widely used theraputic intervention for OSA. A specialized mask which is connected to a breathing machine, is strapped on to the patient's face prior to sleep. The machine then pumps a controlled stream of air through the mask. There are several forms of positive airway pressure available: CPAP (continuous positive airway pressure), VPAP (variable positive airway pressure) and APAP (automatic positive airway pressure).
The sleep specialist will titrate the settings on the breathing machine taking into consideration the pressures required to keep the upper airways opened during sleep, as well as the comfort of the patient (high pressure delivered can be rather uncomfortable).
Surgery:
Surgery is performed with the aim of improving the size or tone of the patient's airway.
Types of possible surgery include:
• Nasal surgery (eg. turbinectomy, correction of a deviated nasal septum)
• Tonsillectomy, adenoidectomy (if these are found to be enlarged and causing obstruction)
• Uvulopalatopharyngoplasty (UPPP), laser-assisted uvulopalatoplasty
• Genioglossus advancement, hyoid suspension, maxillomandibular advancement
Further Reading
The article above is meant to provide general information and does not replace a doctor's consultation.
Please see your doctor for professional advice.
