Haemorrhoids (Piles)
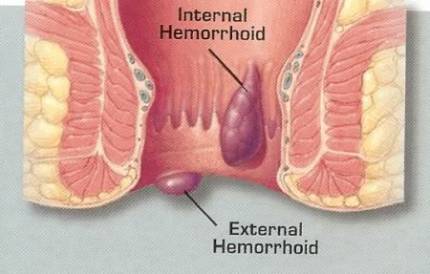
Haemorrhoids, also known as piles, is a common ano-rectal condition typically developing between the ages of 20 and 50. Up to 50% of people above the age of 50 suffer from hemorrhoids to some degree or other. It is basically a condition in which the veins around the anus and lower rectum become swollen and inflammed.
 Haemorrhoids are classified either as being:
Haemorrhoids are classified either as being:
1. Internal – where the hemorrhoids occur inside the rectum. These are generally painless as there are no pain receptors in this region, and most people are unaware of their presence. They occasionally bleed when the veins rupture due to excessive straining or the passage of hard stools.
2. External – where they occur below the anal verge (where pain receptors are present). These tend to be visible and a lump may be felt. External haemorrhoids are prone to thrombosis (blot clot forms inside the pile). When this happens, sudden pain is experienced.
Haemorrhoids are also classified according to their degree of prolapse:
• Grade I – internal haemorrhoids, not prolapsed.
• Grade II – piles are pushed out (prolapsed) on straining, but spontaneously reduce.
• Grade III – piles prolapse on straining, and have to be pushed back manually.
• Grade IV – piles are prolapsed and cannot be manually reduced.
WHAT ARE THE SYMPTOMS?
Bleeding is the earliest symptom. At first, it is minimal fresh bleeding, occurring during defaecation as a “splash in the pan”, or seen on the toilet paper after wiping.
Prolapse is a much later symptom, progressing from Grade II to IV if the underlying cause is not managed. Prolapsed piles can become trapped outside the anal opening if the anal sphincter muscle goes into spasm. Should this happen, blood supply to the haemorrhoid, gets cut off and the pile becomes strangulated.
External haemorrhoids can cause irritation to the skin resulting in itching. As mentioned earlier, external piles can become thrombosed causing significant pain.
WHAT CAUSES PILES?
In general, anything that causes frequent, sustained increase in pressure in the ano-rectal region, can cause haemorrhoids to develop. They include:
• Spending a long time sitting or squatting during defaecation.
• Excessive straining due to constipation.
• Pregnancy and childbirth.
• Obesity
• Portal Hypertension – causing increased back pressure to the rectal veins.
PREVENTING PILES
Ensure you drink sufficient fluids, take in more fibre, exercise and establish regular bowel movement habits, all to help prevent constipation. This is especially so during advanced pregnancy. Sometimes, medication may be required to ensure smooth passage of stools.
Do not spend too long sitting at the toilet bowl during defaecation. Be as efficient as possible.
There is some evidence which suggests that squatting commodes are better than the sitting ones in reducing or preventing haemorrhoids.
DIAGNOSIS
Haemorrhoids can be diagnosed via a thorough physical examination by your doctor. External haemorrhoids may be clearly visible. Internal hemorrhoids require insertion of a proctoscope for visualization, as being soft, internal piles cannot be felt by an examining finger.
It is worth remembering that not all bleeding during defaecation is due to piles. It may be a sign of something more sinister, such as colon cancer, which may co-exist or exist independently of piles. Hence, your doctor may advise for you to have a colonoscopy to exclude more serious conditions in your colon, if you have:
• Signs and symptoms of a more sinister cause
• Risk factors for colon cancer, such a a positive family history
• You are above 50 years of age (or younger in high risk groups) presenting with rectal bleeding
HOW ARE PILES TREATED?
Home Remedies
• Increase fluid and fibre intake to prevent constipation
• Warm Sitz baths, several times a day to soothe painful, inflammed external piles. Sit in a tub filled a few inches of warm water 3 times a day and after each bowel movement for at least 15 minutes. Thoroughly dry the skin after each session.
Medication
• To treat and prevent constipation
• Topical creams, ointments and suppositories to reduce inflammation and discomfort
• Oral medication to shrink the hemorrhoids
• Oral medication to manage pain and inflammation eg. Non-steroidal anti-inflammatory drugs
Surgical Treatment
Thrombosed piles can be treated with a simple excision to bring quick relief.
 Rubber band ligation – tiny rubber bands are placed at the base of the internal pile to cut off its blood supply. The pile withers and falls off after a few days. This procedure is generally not painful (though may be a little uncomfortable) because it is placed in a region devoid of pain receptors.
Rubber band ligation – tiny rubber bands are placed at the base of the internal pile to cut off its blood supply. The pile withers and falls off after a few days. This procedure is generally not painful (though may be a little uncomfortable) because it is placed in a region devoid of pain receptors.
Injection (sclerotherapy) – chemicals are injected into the pile to cause it shrink. Also generally a painless procedure.
Hemorrhoidectomy – surgical excision of the pile is recommended for severe hemorrhoids.
Stapled haemorrhoidectomy – resection of soft tissue above the dentate line, thus disrupting blood flow to the hemorrhoid. Much less painful than traditional hemorrhoidectomy and has faster recovery time.
Transanal Haemorrhoidal Dearterialisation (THD) – a precise, ultrasound-guided ligation of the blood vessels which supply the piles. Much less painful than traditional hemorrhoidectory with shorter downtime.
So, if you think you may have piles, do consult your doctor. Once he has excluded more serious conditions, he will be able to recommend the most appropriate treatment for you, depending on the nature and type of haemorrhoids you have.
Further Reading
The article above is meant to provide general information and does not replace a doctor's consultation.
Please see your doctor for professional advice.
